- Bone infections
- Limb threatening foot infections
- Cellulitis
- And even gangrene
We are proud to provide patients with various treatment options to address your diabetic foot ulcer. Dr. Jam, a diabetic foot specialist, works closely with each patient to develop a treatment plan that matches their needs and gets them back up on their feet. Visit the best podiatrist Los Angeles has today!




What Is a Diabetic Foot Ulcer?
Diabetic foot ulcers are a result of skin tissue breaking down and beginning to expose the lower layers. Typically, they appear in diabetic patients who might have not properly controlled their condition. Constantly treating and addressing diabetes can be challenging, and even a small slipup might be enough to allow an ulcer to develop.
Most often, they form either on your big toes or the balls of the feet. If left untreated, they progressively worse until they can affect the bones beneath the skin. That is why we recommend receiving treatment as soon as you feel one beginning to develop! The sooner you treat a diabetic foot ulcer, the easier it will be.
What is a Foot Wound?
Symptoms of Diabetic Foot:
- Decreased blood flow to the feet
- Decreased healing ability in the feet
- Tingling and/or numbness of the feet
- Decreased ability to fight off infections in the feet
- Loss of sensation in the feet
- Loss of pulses in the feet
What Is So Dangerous About a Diabetic Foot Ulcer?
Complications of Diabetic Foot:
- A loss of feeling in your feet.
- Foot ulcers or sores that do not heal.
- Dry Cracks in the Skin.
- Ingrown Nails or Fungal Nails.
- Swelling.
- Corns and calluses.
- Amputation.
Although amputation is not always required, over 65,000 amputations are performed each year due to complications from diabetes, making it a very real complication. By regularly visiting a specialist in your diabetes foot care you can reduce the risk of lower limb amputation by up to 85%.
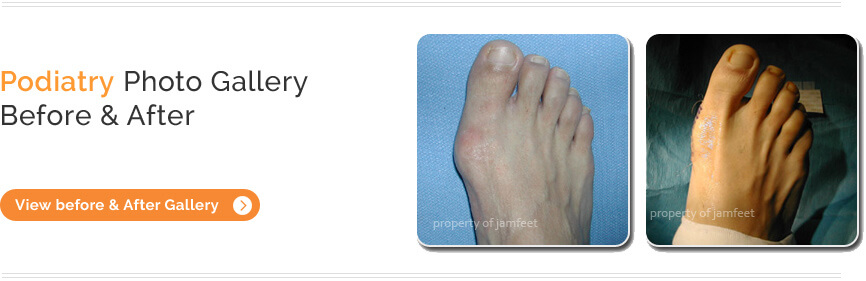
Where Do Diabetic Foot Ulcers Form?
- Your big toes
- The balls of the feet
- Areas associated with bony prominences like over bunions
- On top of hammertoes
- Under a skin callus
What Happens if a Foot Ulcer Is Not Treated?
- Become infected
- Cause bone infection (osteomyelitis)
- Lead to a limb-threatening or foot threatening infection
- A dark callus
- Bleeding
- A callus that is thick or uncomfortable
What Are My Diabetic Foot Ulcer Treatment Options?
Treating a foot ulcer takes two forms: prevention and restoration.
When you visit Dr. Jamfeet, we will work with you to develop a personalized treatment plan. Each treatment focuses on addressing your unique concerns, including:
- Location of the ulcer
- Your current health
- Whether the ulcer is infected
Hyperbaric Oxygen Therapy for Foot Ulceration (HBO Therapy)
Foot Protection
- Diabetic Shoes
- Casts
- Compression Wraps
- Foot Braces
- Custom Shoe Inserts
Infection Prevention
If you have a diabetic foot ulcer, it is vital to prevent infection. Once infected, they become much more serious and more challenging to treat. This is why it is crucial to seek treatment as soon as you think you might have an ulcer.
Ways we might help prevent infection from occuring include:
- Skin disinfection
- Foot baths
- Enzyme treatments
- Dressing it with anti-bacterial wraps
Treating Infected Tissue
Medication: In some cases, antibiotics may be enough to deal with an infected ulcer. We will take a sample of the infected tissue to determine if this treatment is best. Other medications include antiplatelets and anti-clotting drugs.
Debridement: This treatment removes the dead skin, foreign material, and infections that may have been the ulcer’s initial cause.
How Do I Know I Have a Diabetic Foot Ulcer?
One of the earliest signs is drainage from your foot. You might notice leakage in your socks or shoes, or some stains in your socks. Other signs of drainage are odors coming from the affected foot.
You may also notice swelling, redness, or irritation in the affected foot. These usually start out quite mild but quickly develop into constant noticeable discomfort.
This is a visible sign of a foot ulcer that has become quite serious. If you see any blackened tissue on your foot around the ulcer, we advise immediate treatment from a specialist. It could be the beginnings of gangrene, which could result in severe complications.
Factors That Increase Your Risk
- Poorly-fitted shoes
- Insufficient hygiene
- Higher levels of alcohol or tobacco usage
- Heart or kidney disease
- Obesity
- Eye disease from diabetes
- Improper trimming of toenails or calluses by a non-professional
- Poorly controlled Diabetes
- Diabetic Neuropathy
The Podiatrist’s Role in Diabetic Foot:
Podiatrists are an important part of providing appropriate care for people with diabetes. Most podiatrists and specialists recommend annual examinations at a minimum, although for patients at higher risk, more frequent screenings may be necessary.
- Diabetics with no risk -> yearly foot examinations are fine.
- Diabetics with some risk factors -> twice a year screenings at a minimum
- Diabetics with existing foot problems (ulcers, corns, etc…) -> should be seen frequently
- Diabetics with new acute symptoms or problems -> should be seen immediately.