Toenail Fungus Los Angeles – Fungus Treatment Beverly Hills
Warm weather and long days can often serve as an enticement to walk around barefoot. Unfortunately, doing so in unclean public areas can easily result in the development of one or more plantar warts. Like other warts, plantar warts develop as the result of a virus. The human papillomavirus (HPV) enters the skin through tiny cuts or abrasions that may not even be visible to the naked eye. When the virus causes a wart to develop on the sole of the foot, these are considered plantar warts. Warts on other parts of the foot are not considered plantar warts, although the treatment is usually similar. If you have developed a plantar wart in Los Angeles, you should seek treatment from an experienced Board Certified podiatrist like Dr. Jamshidinia. He can help remove your plantar wart safely and effectively.
- 1.Toe nail fungus has been found to affect 2-18% of the worldwide population.
- 2.This percentage translates to 35 million people worldwide who have experienced fungal infections.
- 3.The likelihood of getting toenail fungus increases as you age.
- 4.25% of adults will experience some type of nail fungus by the time that they are 40 years old.
- 5.For senior citizens, the fungus statistics is even higher with 50% of seniors having some type of toe nail fungus.
- 6.One dermatology study in the U.S. found that almost 50% of the people who came into a doctor’s clinic were coming for fungus related problems.
Toenail fungus is much more common than hand nail fungus, because fungi like to live in dark, warm places – and your feet give it that opportunity while being trapped inside your shoes all day. The high rate of toe nail fungus should actually reassure anyone suffering from this problem. While nail fungus is often unsightly and can be painful, it is very common and highly treatable. One reason that so many people ignore the infection is that it can be present for years without ever causing pain. Its prevalence rises sharply among older adults (20 to 30 percent, the studies say, though podiatric physicians think it’s much higher). Because the older adults may be experiencing much more serious medical problems, it is understandable that fungal nails can be passed over as very minor, though it is anything but that.
Whatever the case, the disease, characterized by a change in a toenail’s color, is often considered nothing more than a mere blemish — ugly and embarrassing. It is apparently assumed that since white markings or a darkening of the nail are minor occurrences, the change represents something minor as well, even when the blemish spreads. It may be that cosmetologists see this condition as often as doctors. Nail polish is an easy solution for many women, rendering the problem “out of sight, out of mind.”.
Why Choose Dr. Jamshidinia?
Dr. Jamshidinia at Tower Foot and Ankle Surgery is a board certified foot surgeon trained in all areas of foot and ankle surgery. He is Board Certified by the American Board of Podiatric Surgery.
- 1.American Board of Podiatric Surgery Fellow
- 2.American College of Foot and Ankle Surgeons
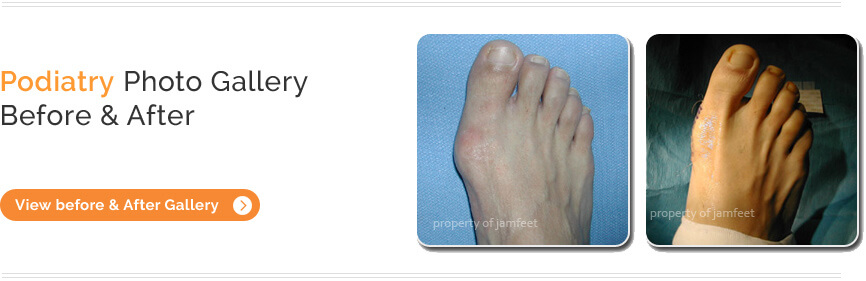
- 3.Thousands of Before/after pictures
- 4.Watch video testimonials from real patients
What is a Fungal Nail?
Onychomycosis is an infection of the bed and plate underlying the surface of the nail, and is caused by various types of fungi, which are commonly found throughout the environment. Fungi are simple parasitic plant organisms, such as molds and mildew, which lack chlorophyll and therefore do not require sunlight for growth. A group of fungi called dermophytes easily attack the nail, thriving off keratin, the nail’s protein substance.
When the tiny organisms take hold, the nail may become thicker, yellowish-brown or darker in color, and foul smelling. Debris may collect beneath the nail plate, white marks frequently appear on the nail plate, and the infection is capable of spreading to other toenails, the skin, or even the fingernails.
Because it is difficult to avoid contact with microscopic organisms like fungi, the toenails are especially vulnerable around damp areas where people are likely to be walking barefoot — swimming pools, locker rooms, and showers, for example. Injury to the nail bed may make it more susceptible to all types of infection, including fungal infection. Those who suffer chronic diseases, such as diabetes, circulatory problems, or immune-deficiency conditions, are especially prone to fungal nails. Other contributory factors may be a history of athlete’s foot and excessive perspiration.
Prevention of Toenail Fungus:
Proper hygiene and regular inspection of the feet and toes are the first lines of defense against fungal nails. Clean and dry feet resist disease.
- Wash your feet with soap and water, remembering to dry thoroughly.
- Wear shower shoes when possible in public areas.
- Change shoes, socks, or hosiery more than once daily.
- Clip toenails straight across so that the nail does not extend beyond the tip of the toe.
- Wear shoes that fit well and are made of materials that breathe.
- Avoid wearing excessively tight hosiery to decrease moisture.
- Wear socks made of synthetic fiber that “wicks” moisture away from your feet faster than cotton or wool socks do.
- Disinfect instruments used to cut nails.
- Disinfect home pedicure tools.
- Don’t apply polish to nails suspected of infection (those that are discolored, for example).
Because fungi are everywhere, including the skin, they can be present for months before signs of infection appear. By following precautions, including proper hygiene and regular inspection of the feet and toes, chances of the problem occurring can be sharply reduced, or even put to a halt.
Artificial Nails and Polish
Moisture collecting underneath the surface of the toenail would ordinarily evaporate, passing through the porous structure of the nail. The presence of an artificial nail or a polish impedes that, and the water trapped below can become stagnant and unhealthy, ideal for fungi and similar organisms to thrive.
Always use preventive measures when applying polishes. Disinfect home pedicure tools and don’t apply polish to nails suspected of infection those on toes that are red, discolored, or swollen, for example.
Treatment
Once you are diagnosed with having a fungal toenail infection, you can proceed to treatment. Toenail fungus is a highly common problem in the US, and one that can be treated in many different ways depending on the severity of your case.
Treatment methods for nail fungus include:
- 1.Over the counter antifungal medications
- 2.Prescription antifungal medicines
- 3.Natural Home Remedies like Tea Tree Oil, Vinegar, Epsom Salt, etc…
- 4.A daily routine of cleansing may temporarily suppress mild infections.
- 5.White markings that appear on the surface of the nail can be filed off, followed by the application of an over-the-counter liquid antifungal agent.
The different treatment options each have their own advantages and disadvantages. However, even the best over-the-counter treatments may not prevent a fungal infection from coming back. A fungus may work its way through the entire nail, penetrating both the nail plate and the nail bed. If an infection is not overcome, or continues to reappear, further medical attention will be needed to completely cure the infected toenail(s).
Podiatric Toenail Fungus Treatment
A podiatrist can detect a fungal infection early, culture the nail, determine the cause, and form a suitable treatment plan, which may include prescribing topical or oral medication, and debridement (removal of diseased nail matter and debris) of an infected nail. Indeed, debridement is one of the most common foot care procedures performed by DPMs.
Newer oral antifungals approved by the Food and Drug Administration may be the most effective treatment. They offer a shorter treatment outlook (three to four months) and improved effectiveness, though DPMs advise that lengthier treatments, up to 12 months, may still be required for some infections. Current studies show that, for a small percentage of the population, there are some unwanted side effects with any oral antifungal.
In some cases, surgical treatment may be required. Temporary removal of the infected nail can be performed to permit direct application of a topical antifungal. Permanent removal of a chronically painful nail, which has not responded to any other treatment, permits the fungal infection to be cured, and prevents the return of a deformed nail.
Trying to solve the infection without the qualified help of a podiatric physician can lead to more problems. With new technological advances in combination with simple preventive measures, the treatment of this lightly regarded health problem can often be successful.
Toenail Fungus -Frequently Asked Questions:
The laser is a specially designed, patented device that shines through your toenail and vaporizes the fungus embedded in your nail bed and nail plate that causes toenail fungus. The laser is tuned to a frequency that affects only those cells responsible for the nail infection. This treatment is brand new to the United States and is available at less than 100 doctor’s offices nationwide given this recent breakthrough. See video for more details.
The laser light beam has no effect on healthy tissue. Patients should experience no discomfort during or after the treatment.
Pts will experience some warming of the nail which will not be painful or cause any discomfort. The patient will also sometimes experience a spray of cooling agent which will cool any discomfort immediately.
Pts will experience some warming of the nail which will not be painful or cause any discomfort. The patient will also sometimes experience a spray of cooling agent which will cool any discomfort immediately.
Our clinical studies to date reveal that over 88% of treated patients show significant improvement. In most cases the nail fungus pathogen is completely eliminated..